Screening Tools & Measurement Guides
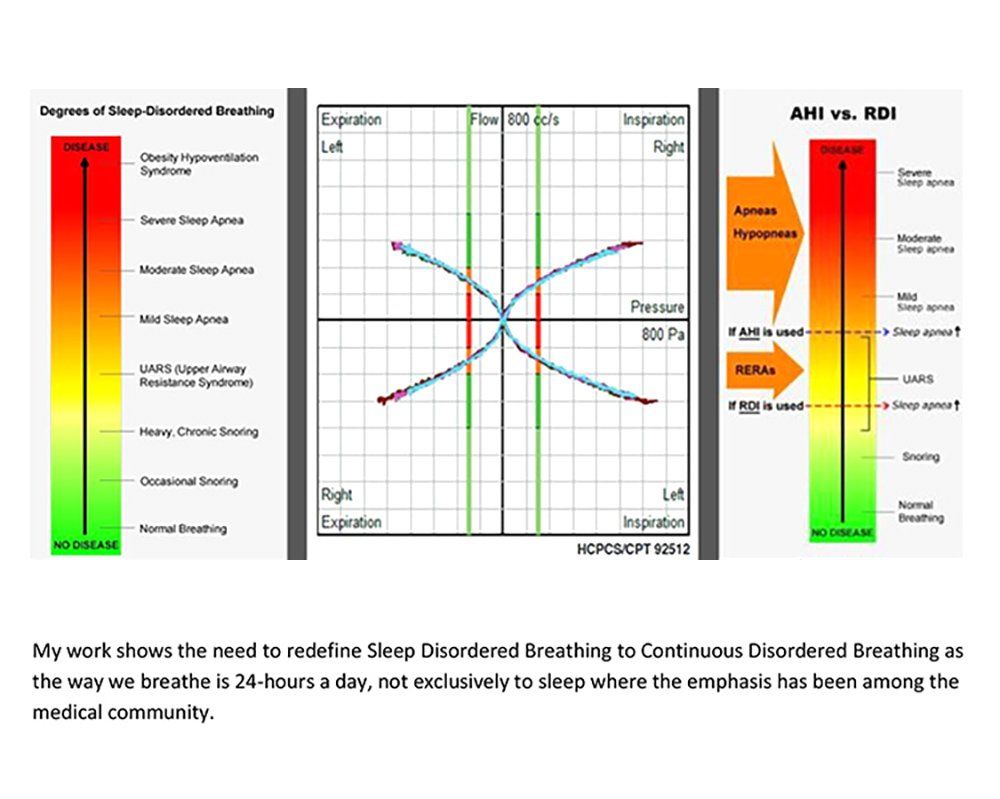
Nasal Flow & Disease Progression
| Scale | Log 10R (VR, REFF) | Flow (ccm/s) | Obstruction, Resistance (NR6) | Disease Progression Scale |
|---|---|---|---|---|
| 1 | < = 0.75 | >500 | Very Low | Normal Breathing |
| 2 | 0.75 - 1.00 | 300 - 500 | Low | Snoring May Occur |
| 3 | 1.00 - 1.25 | 180 - 300 | Moderate | Chronic to Heavy Snoring RDI-RERAS-UARS |
| 4 | 1.00 - 1.50 | 60 - 180 | High | Mild to Moderate OSA |
| 5 | >1.50 | <60 | Very High | Hypoventilation (AHI)-Severe OSA |
Nasal Volume Normal Values & Ranges
G: Girls | B: Boys
| Age (Years) | MCA (cm² L+R/2) | Distance 0-3 cm³ Decongested | Distance 0-5 cm³ Decongested | Distance 2-5 cm³ Decongested (most sensitive for patency) | Measurement Considerations |
|---|---|---|---|---|---|
| Neonates | 0.33 | 0.44 | 1.19 | NA | No second notch or MCA2 noted |
| 1 | 0.43 | 0.63 | 1.05 | NA | No second notch or MCA2 noted |
| 2 | 0.27 | 0.75 | 2.14 | NA | |
| 3 | 0.31 | 0.76 | 2.59 | NA | |
| 4 | 0.30 | 0.77 | 2.86 | 2.43 | |
| 5 | 0.32 | 0.88 | 2.89 | 2.49 | |
| 6 | 0.35 | 0.90-1.43 | 2.92 | 2.52 | |
| 7 | 0.38 | 0.90-1.43 | 2.95 | 2.55 | |
| 8 | 0.39 G | 0.37 B | 0.90-1.43 | 3.00 | 2.56-2.59 | |
| 9 | 0.43 G | 0345 B | 0.89-1.40 | 3.36-4.89 | 2.62 | Decongestion will increase NV by 16% |
| 10 | 0.46 G | 0.41 B | 0.89-1.40 | 3.36-4.89 | 2.66 | |
| 11 | 0.39 G | 0.42 B | 1.01-1.52 | 3.36-4.89 | 2.70 | Natural decrease in volume occurs |
| 12 | 0.48 G | 0.50 B | 1.01-1.52 | 3.49- | 2.73 | MCA changes significant for girls 11-13 |
| 13 | 0.53 G | 0.52 B | 1.11-1.58 | Varies with growth | 2.76 | Age will vary with growth, but the average increase is 0.32cm³ |
| 14 | 0.52 G | 0.55 B | 1.11-1.58 | Varies with growth | 3.58-3.84 | The MCA (CSA) becomes larger in boys |
| 15 | 0.50 G | 0.54 B | 1.14-1.80 | Varies with growth | 3.58-3.84 | MCA changes significant for boys 15-17 |
| 16 | 0.53 G | 0.61 B | 1.14-1.80 | Varies with growth | 3.58-3.84 | |
| 17 | 0.58 G | 0.70 B | 1.19-1.88 | Varies with growth | 4.16 | May not reach full adult volume size in males at 17 years old. |
| >18 | 0.73 | 1.24-1.91 | 6.01-8.14 | 4.48 |
Adults
| Age (Years) | MCA (cm² L+R/2) | Distance 0-3 cm³ Congested | Distance 0-3 cm³ Decongested | Distance 2-5 cm³ Congested | Distance 2-5 cm³ Deongested | Distance 0-5 cm³ Congested | Distance 0-5 cm³ Decongested | Measurement Considerations |
|---|---|---|---|---|---|---|---|---|
| 19+ | 0.73 | 1.80-3.34 M | 1.96-3.10 F | 2.41-3.97 M | 2.47-3.73 F | 2.95-6.47 M | 3.09-5.77 | 4.06-8.76 M | 4.72-8.40 F | 6.01-6.43 | 7.62-8.14 | Congested MCA 0.41-0.67 |
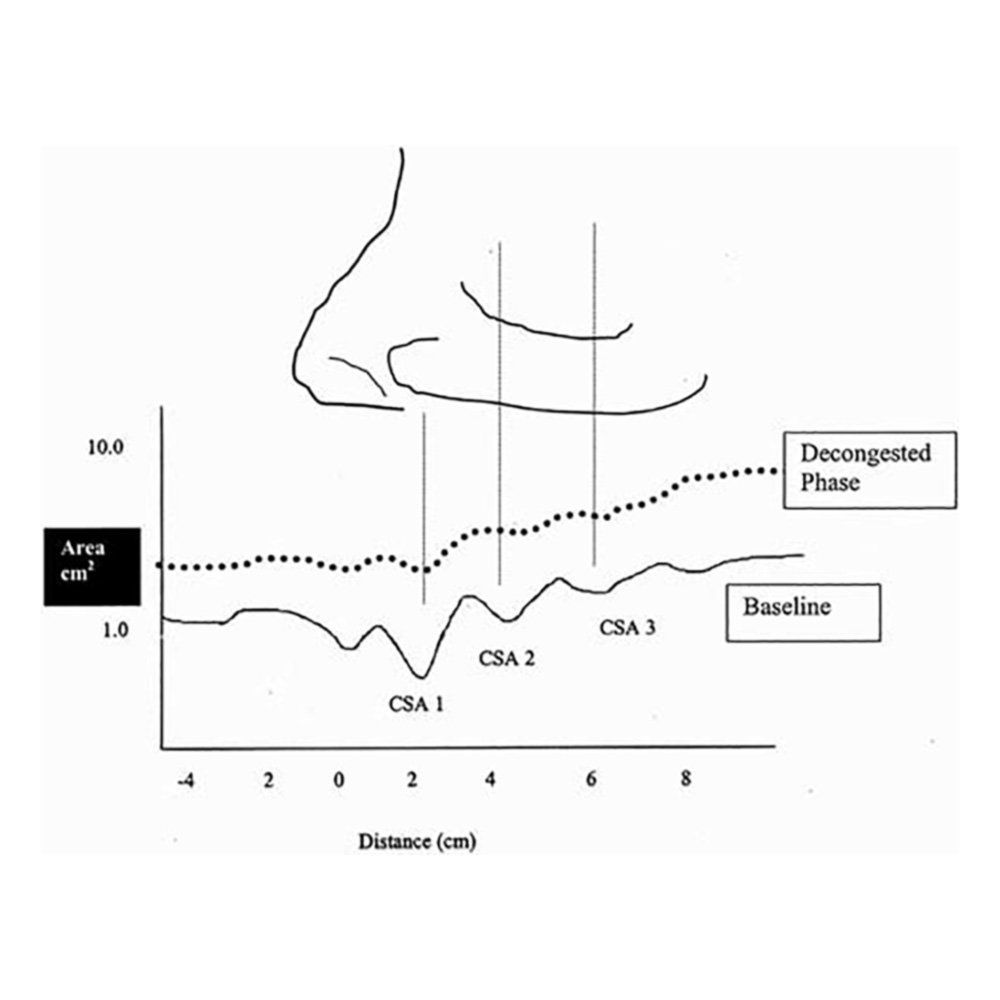
| ~20% increase in nasal volume | ~25% increase in nasal volume | Decongestion at MCA2 opens up with decongestion up to 35% |
Disclaimer: This website is not a sole source in determining patient healthcare outcomes and should not be exclusive without a physical exam, patient questionnaire, patient interview of symptoms, or additional diagnostics completed by a licensed healthcare provider. The website is for information and educational purposes to show how nasal airway measurements allow the HCP to objectively quantify the patency of the nasal away and its part in airflow limitations. It is not medical advice, but based on evidenced based medicine, nasal aerodynamic studies, and validated research over 20+ years using the noninvasive technology methods. The noninvasive, objective nasal measurement processes do not diagnosis a breathing disorder, but allow the HCP to screen and understand how the treatment options are helping for better results towards nasal breathing. Additional questions and educational assistance on the methods, processes for results, and the theory of nasal aerodynamics may be sent through our website query.
Citations provided by request only.